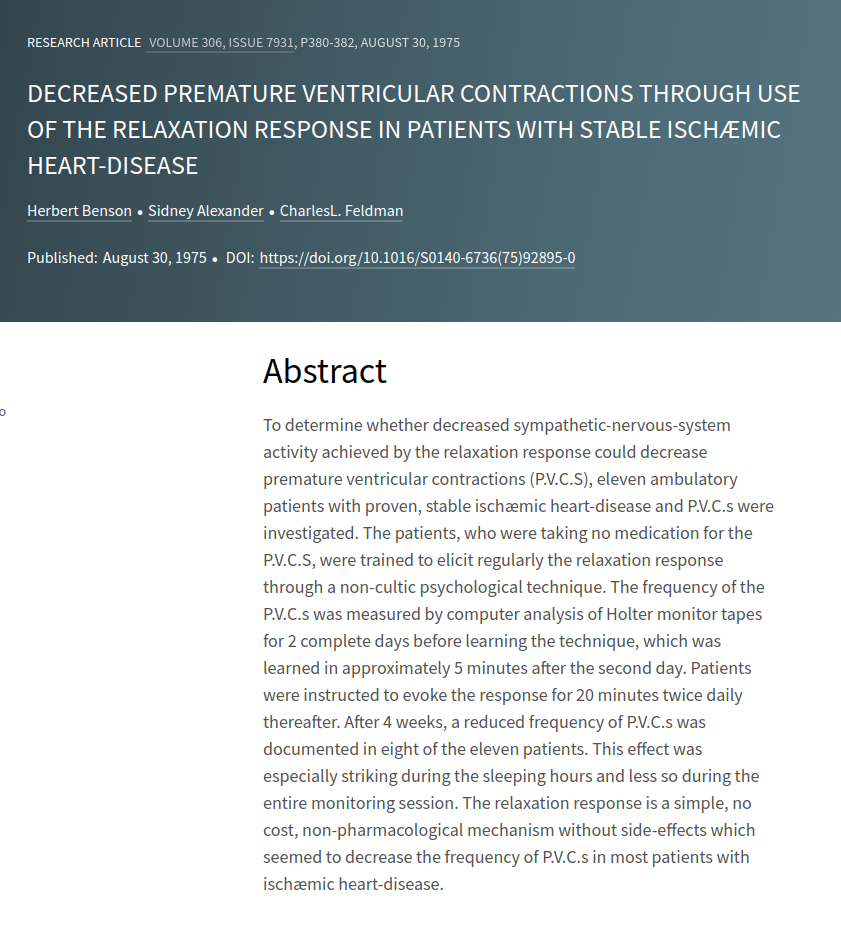
To determine whether decreased sympathetic-nervous-system activity achieved by the relaxation response could decrease premature ventricular contractions (P.V.C.S), eleven ambulatory patients with proven, stable ischæmic heart-disease and P.V.C.s were investigated. The patients, who were taking no medication for the P.V.C.S, were trained to elicit regularly the relaxation response through a non-cultic psychological technique. The frequency of the P.V.C.s was measured by computer analysis of Holter monitor tapes for 2 complete days before learning the technique, which was learned in approximately 5 minutes after the second day. Patients were instructed to evoke the response for 20 minutes twice daily thereafter. After 4 weeks, a reduced frequency of P.V.C.s was documented in eight of the eleven patients. This effect was especially striking during the sleeping hours and less so during the entire monitoring session. The relaxation response is a simple, no cost, non-pharmacological mechanism without side-effects which seemed to decrease the frequency of P.V.C.s in most patients with ischæmic heart-disease.
Decreased Premature Ventricular Contractions Through Use of the Relaxation Response in Patients with Stable Ischemic Heart-Disease
Publication
The Lancet
306(7931), p. 380-382
Abstract
Web and Email Links
Related Listings
Journal
Neuroreport
Meditation is a conscious mental process that induces a set of integrated physiologic changes termed the relaxation response. Functional magnetic resonance imaging (fMRI) was used to identify and characterize the brain regions that are active during a simple form of meditation. Significant (p<10(-7)) signal increases were observed in the group-averaged data in the dorsolateral prefrontal and parietal cortices, hippocampus/parahippocampus, temporal lobe, pregenual anterior cingulate […]
Journal
Nature
Since meditative practices are associated with changes that are consistent with decreased activity of the sympathetic nervous system, it is conceivable that measurable body temperature changes accompany advanced meditative states. With the help of H.H. the Dalai Lama, we have investigated such a possibility on three practitioners of the advanced Tibetan Buddhist meditational practice known as g Tum-mo (heat) yoga living in Upper Dharamsala, India. We report here that in a study perfor […]
Journal
Journal of Cardiopulmonary Rehabilitation
We previously reported reduced blood pressure, psychological symptoms, and other cardiac risk factors in hypertensive patients who participated in a nonpharmacologic, outpatient behavioral program. The present study is a 3 to 5 year follow-up of 59 (60%) of the same patients (who served as their own controls) to assess continued efficacy of the program. At entry into the study, patients had hypertension for a median of 6 years. Therefore, it is unlikely that placebo effect could expla […]